|
The single most important factor in getting your medical aid claims paid quickly
is accuracy of information. That may sound obvious, but in reality
many claims are delayed due to inaccurate details being supplied. Most
claims are assessed automatically by computers these days, and computers require
100% accuracy. Inaccurate claims may be delayed because they require human
intervention, or they may be rejected altogether.
Panacea will automatically verify the membership details of the medical aid
patients that you capture. This will enable you to identify incorrect
membership details before you send eClaims, saving you a lot of time and hassle.
It also helps to prevent fraud. The verification process is very quick and
will usually be completed within seconds of you capturing a new account.
This means that the patient will probably still be sitting in the waiting room,
enabling you to rectify the problem immediately.
 After you save a new account, Panacea will verify all
the beneficiaries on the account. If it finds a problem with any of the details
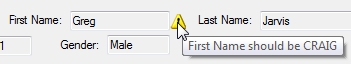
it will display a small yellow triangle next to the relevant field. If you
move your mouse over the triangle it will display a message indicating what the
problem is.
After you save a new account, Panacea will verify all
the beneficiaries on the account. If it finds a problem with any of the details
it will display a small yellow triangle next to the relevant field. If you
move your mouse over the triangle it will display a message indicating what the
problem is.
Panacea can also make helpful suggestions on how to correct
the data. In fact, if you click Auto Correct Member or
Auto Correct Beneficiary Panacea will actually make the necessary
corrections for you.
Certain medical aids also provide additional information during the verification process, such as authorizations and benefit information. This saves you having to call their call centre.
|